Main menu
You are here
Lasik eye surgery retinal detachment
Lasik eye surgery retinal detachment
Abstract
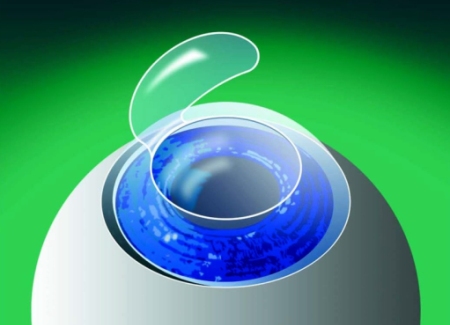
Aim: To assess the efficacy and safety of laser in situ keratomileusis (LASIK) for correction of myopic refractive errors in eyes which have previously undergone retinal detachment surgery.
Methods: In a prospective, non-comparative case series, 10 eyes of nine patients who had a myopic refractive error and had previously undergone retinal detachment surgery underwent LASIK surgery according to the standard
surgical protocol. The surgery could be completed in eight eyes and in two eyes it was aborted intraoperatively. The parameters evaluated included the uncorrected visual acuity, best corrected visual acuity, refraction, detailed fundus evaluation with indirect ophthalmoscope, slit lamp biomicroscopy, and corneal pachymetry. Any intraoperative or postoperative complications were
recorded. Follow up visits were scheduled at day 1, 1 week, 1 month, 3 months, and 6 months after LASIK.
Results: Eight eyes underwent successful LASIK surgery. The mean spherical equivalent before surgery was −5.436 (SD 1.6) dioptres (D), which was reduced to +0.42 (0.65) D, −0.07 (1.32) D, −0.06 (1.39) D, and −0.06 (0.65) at 1 week, 1 month, 3 months, and 6 months respectively after LASIK. The uncorrected visual acuity improved in all the eyes and the best corrected visual acuity improved or remained same in all the eyes. There was no retinal complication after LASIK.
Conclusion: LASIK may be used to correct refractive errors in eyes that have undergone retinal detachment surgery. However, scarred conjunctiva in such cases may prevent generation of optimal suction for the microkeratome.
Keywords: LASIK, retinal detachment surgery
* Other Sections▼
o Abstract
o METHODS
o RESULTS
o DISCUSSION
o REFERENCES
Myopic refractive errors are common in eyes that develop a retinal detachment.1, 2 In addition, myopic changes may also be induced by retinal detachment surgery because of the changes in axial length, anterior chamber depth, or position of the crystalline lens.3, 4 Thus, many patients demand a refractive correction after undergoing retinal detachment surgery.
LASIK (laser in situ keratomileusis) has gained wide acceptance as the procedure of choice for the correction of a wide variety of refractive errors. It has also been found useful in treating refractive errors in eyes that have undergone previous ocular surgery.5–7 However, the efficacy of LASIK has not been evaluated for correction of refractive errors after retinal detachment surgery. We therefore undertook the present study to evaluate the safety and efficacy of LASIK in eyes that have undergone a retinal detachment surgery.
* Other Sections▼
o Abstract
o METHODS
o RESULTS
o DISCUSSION
o REFERENCES
METHODS
For the present prospective study, 10 eyes of nine patients with a myopic refractive error were enrolled from the retina service of a tertiary care eye hospital. All these patients had undergone a conventional retinal detachment surgery for primary rhegmatogenous retinal detachment with application of a scleral buckle and encirclage, at least 6 months before inclusion in the study.
A complete ocular and medical history was obtained in all patients. Patients who were not willing to wear spectacles or contact lenses were included in the present study. Written consent was obtained after detailed instruction and discussion with the patient. Preoperative evaluation included the measurement of the uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA), cycloplegic refraction, slit lamp biomicroscopy, indirect ophthalmoscopy, ultrasonic pachymetry, applanation tonometry, and videokeratography. The mean preoperative Sim K on Orbscan topography system (Bausch and Lomb, Salt Lake City, UT, USA) was 43.02 (SD 2.22). Intraoperative evaluation included measurement of the flap thickness using the Corneo Gage plus (Sonogage Inc, Cleveland, OH, USA) ultrasonic pachymeter. The central corneal thickness was measured just before initiating the surgery and then after lifting the stromal flap, before laser ablation.
Surgery was performed under topical anaesthesia (0.5% oxybuprocaine (proparacaine)). The hansatome microkeratome (Chiron Vision, Claremont, CA, USA) was used to create a superiorly hinged flap. The hansatome head cutting a 180 μm flap and an 8.5 mm suction ring was used in all the cases. The intraocular pressure generated after activation of the suction was measured with the Barraquer tonometer. The flap was cut only if on applanation of the cornea, the central mire was equal to or within the circular mark etched on the tonometer (indicating a pressure of equal to or more than 65 mm Hg). Standard surgical technique was used and the Chiron Technolas 217 excimer laser (Chiron Vision, Claremont, CA, USA) was used for laser ablation. The optic zone diameter was 5.5 mm in all the cases and a minimal residual stromal thickness of 250 μm was left after laser ablation in all the eyes. The target refraction was emmetropia in all the operated eyes. In two eyes with extensive conjunctival scarring adequate suction could not be obtained and the IOP generated was less than 65 mm Hg. Surgery was not performed in these two eyes.
All patients received ciprofloxacin (0.3% four times daily) and fluorometholone (0.1% four times daily) eye drops for 2 weeks and tear supplements for 4 weeks in the postoperative period. Routine postoperative examinations were scheduled at day 1, 1 week, 1 month, 3 months, and 6 months after the surgery. The UCVA, BCVA, refraction, corneal topography, and pachymetry were performed at the 1 week, 1 month, 3 month, and 6 month follow up and any postoperative complication was noted.
* Other Sections▼
o Abstract
o METHODS
o RESULTS
o DISCUSSION
o REFERENCES
RESULTS
Ten eyes of nine patients were enrolled for the present study, out of which eight eyes of seven patients subsequently underwent LASIK surgery for refractive correction after retinal detachment surgery. All patients were male. The right eye was operated in five patients, the left eye in one patient, while one patient had bilateral surgery. The mean age at the time of surgery was 33.29 years (range 21–58 years). The mean time interval from retinal detachment surgery was 10.63 months (range 7–15 months). The indication for retinal detachment surgery was rhegmatogenous retinal detachment associated with myopia in all the patients. All patients were myopic before surgery with a mean spherical equivalent of −5.536 (SD 2.413) D on cycloplegic correction (range −3 to −11D). Postoperatively, the mean spherical equivalent was +0.43 (0.66) D at 1 week, −0.07 (1.32) D at 1 month, −0.067 (1.39) D at 3 months, and −0.06 (0.65) D at 6 months (Fig 11).Figure 1). Four eyes (50%) were within plus or minus 0.5 D of emmetropia at 6 months, while all eight eyes (100%) were within plus or minus 1 D of emmetropia at 6 months after the surgery. The mean refractive cylinder before surgery was −2.14 (1.44) D (range −0.75 D to −3.5 D). A residual refractive cylinder of −0.5 D was present in only one of the eight eyes, 6 months after LASIK.

Figure 1
Mean spherical equivalent (mean spherical deviation from emetropia) shown before and after surgery.
Five out of eight eyes (62.5%) had BCVA of 6/12 or better before surgery, while six eyes (75%) had a BCVA of better than 6/12 after surgery. The preoperative UCVA ranged from 6/24 to 1/60. At final examination at 6 months, four eyes (50%) had a UCVA of equal to or better than 6/12, while all eight eyes (100%) had a UCVA better than or equal to 6/18. There was no decrease in the UCVA or BCVA in any of the eyes in the follow up period
Details of the patients who underwent LASIK after RD surgery
The mean thickness of the flap made by the hansatome was 132.1 (30.26) μm (range 110–170 μm). The mean thickness of ablation was 117.7 (30.48) μm (72.00–135.0 μm). Mean preoperative pachymetry was 527.1 (20.24) μm. Mean postoperative pachymetry at the 1 week, 1 month, 3 month, and 6 month follow up was 386.4 (33.27) μm, 402 (63.60) μm, 425 (65.63) μm, and 430 (64.42) μm respectively. There were no other postoperative complications (Fig 22).Figure 2). All patients were satisfied with the final visual outcome.
 Figure 2
Figure 2
(A) Pre-LASIK topography map. (B) Post-LASIK topography map.
No retinal pathology predisposing to retinal detachment was detected on indirect ophthalmoscopy done preoperatively. On indirect ophthalmoscopy done at 3 months and 6 months after the surgery, none of the eyes was found to have any new retinal lesion and in all the eyes the retina was flat.
* Other Sections▼
o Abstract
o METHODS
o RESULTS
o DISCUSSION
o REFERENCES
DISCUSSION
LASIK is being successfully used for the correction of myopic refractive errors all over the world. The therapeutic value of LASIK has also been realised for the correction of refractive errors after previous surgical procedures such as penetrating keratoplasty, radial keratotomy, and cataract surgery.5–7 However, there are several studies which have reported the occurrence of retinal detachment following LASIK surgery, especially in myopic eyes.8, 9
There is only one study10 in the literature, which has mentioned the use of LASIK for management of refractive errors in eyes following retinal detachment surgery. All eyes operated had an improvement in the uncorrected visual acuity and there was no decrease in the best corrected visual acuity in any of the cases. All eyes achieved a refractive error of within 1 D of emmetropia and an uncorrected visual acuity of better than 20/60. Although there was no retinal complication in the postoperative period, a longer follow up is required with regular screening of the retinal periphery. The only problem we found in doing LASIK after retinal detachment surgery was that these patients have extensive conjunctival scarring, which hampers the function of the suction ring of the microkeratome. Owing to the presence of scar tissue, a good hold on the ocular surface is not obtained and thus suction may be inadequate to initiate the procedure. This can lead to a decrease in the level of intraocular pressure obtained before performing the microkeratome cut which eventually affects the thickness of the flap. Thus, one might see thin flaps in such cases and the suction may be too inadequate even to initiate the surgery, as in two of our cases where an adequate IOP could not be generated to proceed with the microkeratome cut. In such cases a good option can be photorefractive keratectomy or laser epithelial keratomileusis (LASEK).
In conclusion, LASIK may be considered for treating refractive errors post-retinal detachment surgery. In addition, this procedure is especially useful for correction of anisometropia induced by scleral buckling surgery. But there may difficulties in performing the procedure owing to conjunctival scarring and thereby poor suction generation. However, in those cases where it is possible to develop adequate suction one can perform the procedure with reasonable safety and efficacy. Further studies with a larger sample size and longer follow up will be helpful to either validate or refute the results of this study.
source: nlm.nih.gov - Lasik eye surgery retinal detachment

